Getting reliable information about healthcare to everyone who needs it in a timely way is surely a goal we can all agree on. However, it’s still very far from being a reality. Around the world — especially, but by no means exclusively in the Global South — clinicians and healthcare workers, patients and carers, struggle to access accurate and up-to-date information. One small but mighty organization, Healthcare Information for All (HIFA), is trying to change this, by “convening all relevant stakeholders to address this complex challenge”. They’re now seeking to expand those stakeholders through a global consultation survey, open to all, being launched today to coincide with the IFLA conference in Amsterdam. Learn more, including how you can get involved, in this interview with their Global Coordinator, Neil Pakenham-Walsh, who will also be speaking at the conference.
Please can you tell us a bit about HIFA, including the history, purpose, and goals of the organization?
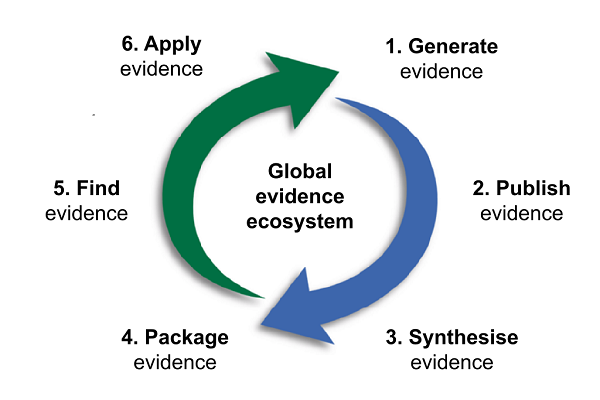
HIFA is a global campaign for a world where every person has access to the information they need to protect their own health and the health of others. It is administered by a small non-profit called Global Healthcare Information Network (GHI-Net), based near Oxford UK. HIFA emerged following the publication of a 2004 Lancet paper, which argued that the global evidence ecosystem isn’t working, due largely to intrinsic weaknesses in the system itself, with consequent and pervasive lack of availability of timely, relevant, reliable healthcare information at all levels of care, especially in low- and middle-income countries. The paper called on the World Health Organization (WHO) to champion the goal of universal access to reliable healthcare information. WHO encouraged GHI-Net to take the lead. Our primary purpose is to champion universal access and strengthen the intrinsic weaknesses — poor communication and coordination, poor understanding, and poor advocacy across the global evidence system — as identified in the Lancet paper. We started with a donation of £2,000 from The BMJ, which we used to develop and launch HIFA in 2006 in Mombasa, Kenya. We were confident that we could make a difference, thanks to the recent emergence of group email communications, which enables us to facilitate in-depth global discussions among thousands of people on a wide range of topics relating to information needs and how to meet them. Our approach is based on Wenger’s ‘community of practice’ concept and, within weeks, enabled us to connect 1,000 professionals representing all parts of the global evidence ecosystem. Our network continues to grow and we now have 20,000 members in 180 countries. Around 500 members have stepped up as volunteers: steering group members, country representatives, a social media team, and project working groups. We currently have 20 projects that aim to promote communication and understanding among HIFA members at large of different aspects of the evidence ecosystem. For example, the project on Information for Prescribers and Users of Medicines worked with the London School of Hygiene and Tropical Medicine to produce this systematic review.
What do you mean by the term ‘reliable healthcare information’?
We use this term to have a wider meaning than it suggests, namely that it is the information people need to protect their own health and the health of others. By definition, such information should not only be accurate and up to date, it should also be unbiased and reflect, as far as possible, the cumulative evidence based on robust research; it should clearly be in the right language, technical level, and format; it should be relevant and applicable to the person’s immediate situation (which is always changing); and the person should be empowered to differentiate it from the barrage of misinformation that does not fulfil these criteria. A few of my colleagues have proposed the term ‘essential healthcare information’, analogous to essential medicines, but I prefer the term ‘reliable’, as defined above, as I don’t believe we can categorize information in the same way as essential medicines. Rather, I see the issue in terms of meeting people’s information needs (both perceived and actual), which will vary from person to person and from one situation to another.
As a co-founder of HIFA, what is your role and how has it changed over the years?
My role is to coordinate the effort. I am responsible for leading others to plan and implement our work. My role has been steady: to strengthen communication among stakeholders, strengthen understanding, and strengthen advocacy — three recognised intrinsic weaknesses of the global evidence ecosystem.
Throughout, the main focus has been on communication. We have moderated countless spontaneous discussions on the full range of topics relating to improving the availability and use of information. We have also supported many planned, deep-dive discussions, typically lasting 4-6 weeks and often leading to publication in peer-reviewed journals. Each of these planned discussions is sponsored by an organization, including two projects supported by WHO, and a further two projects currently supported by large research consortia funded by the Norwegian Research Council, looking at the use of mobile phones by health workers, and the role of civil society in evidence-informed policymaking. They demonstrate the value of HIFA as a low-cost method to harness stakeholder perspectives to complement related research.
To improve understanding of information needs and how to meet them, we have developed and tested a database to collate experiential knowledge expressed by HIFA members. The aim is to complement conventional approaches such as peer-reviewed research and systematic reviews, and to have a more inclusive approach. However, we have been unable to gain the funding we need to maintain this.
We have had more success with advocacy. For example, as a result of our work, the World Medical Association (WMA), representing 10 million doctors, now has an official policy in support of universal access to reliable healthcare information, and has agreed our seven recommendations on the way forward. We have always recognised that we are far too small to make a difference in such a big global health issue on our own, so we have built a community of 445 supporting organizations worldwide. Most importantly we applied and were granted official relations with WHO in 2022.
Why did HIFA choose to focus on equity and what does that mean in practice?
The availability and use of reliable healthcare information is, first and foremost, a human rights issue. It is fundamental to safe and effective care, from the home through all levels of the health system, and has been recognized by HIFA and others as a determinant of the right to health. Reliable healthcare information is a prerequisite for safe and effective care, and for global health equity. HIFA and the New York Law School demonstrated that governments have a legal obligation under international human rights law to ensure that their populations have adequate access to reliable healthcare information, a responsibility that has been flouted with impunity by heads of state, as seen during the COVID-19 pandemic.
People are dying and suffering in huge numbers, due (at least in part) to a lack of availability and use of reliable healthcare information, especially in low- and middle-income countries, where the needs are greatest, and where early homecare decisions by lay people are so important. It is self-evident to me that every person should have access to the information they need to care for themselves and others. Often this information is very basic, such as knowing whether to give more fluids or less fluids to a child with diarrhea. A personal experience – the avoidable death of a child in Peru in 1987 because of the false belief in withholding fluids — was my seminal moment in campaigning for equity in health information.
What do you see as HIFA’s greatest success (or strength) and greatest failure (or weakness) so far?
I am proud of the way that we have grown organically over the years, with each achievement building on the last (see: https://www.hifa.org/about-hifa/achievements). Rather than any one achievement, it is the consistent delivery of achievements that is our greatest success. Our greatest failure is, paradoxically, our inability to fully implement our strategy because we have been unable to attract the resources needed. We always saw the strategy as requiring three professional full time equivalents, and we continue to have only one person and a part-time administrator. In particular, we are missing in-house expertise in organisational development and fundraising.
Looking ahead, what do you see as HIFA’s greatest opportunity (or opportunities) over the next three to five years?
Today efforts are fragmented, and high-level political and financial investment is almost absent. For example, there is no single funder and no government that is committed to universal access to reliable healthcare information. The world’s doctors are the only stakeholder group to have a collective policy declaration on universal access. I predict that all of this is about to change, and I am excited by it.
The driver of change will be WHO. I repeat the clarion call of our Lancet article in 2004. The greatest opportunity that we are focusing on right now is for WHO to explicitly commit to the goal of universal access to reliable healthcare information. This would be a game-changer.
The concept isn’t new to WHO. Universal access is implicit in WHO’s Constitution, published 75 years ago: ‘The extension to all peoples of the benefits of medical, psychological and related knowledge is essential to the fullest attainment of health’.
Throughout its history, WHO has arguably been the world’s leading publisher of health information. However, when I worked there as an editor in 1995, the focus of the staff I talked to was on their role as a publisher and provider of information. There was no initiative to convene stakeholders. This changed to a limited extent in 2000, when I attended the launch of Hinari, an initiative launched by WHO in collaboration with publishers, to improve the availability and affordability of e-journals (and, later, e-books). The initiative has thrived and remains relevant and important. But it only addresses one aspect of the global evidence ecosystem.
“We’re not just fighting an epidemic; we’re fighting an infodemic,” said Dr Tedros, Director-General of WHO at the Munich Security Conference in February 2020. In response WHO set up an Infodemic Management unit and convened social media and tech companies to find solutions. Today it is clear that the concept of universal access is now at the highest levels of WHO as seen, for example in the title of this May 2023 paper co-authored by the Deputy Director-General of WHO Dr Zsuzsanna Jakab: Universal health information is essential for universal health coverage’
I believe there is now unstoppable momentum for WHO to explicitly champion the goal of universal access to reliable healthcare information. WHO normally operates on a process of resolutions being brought by countries and approved at a World Health Assembly, but universal access is already included in its Constitution, and the organisation has endorsed previous initiatives that align with universal access.
How will you make this a reality – what are the biggest challenges/barriers?
We have taken the first steps by becoming an NGO in official relations with WHO in 2022. We have agreed a collaboration plan with WHO. Our plan in 2024 and beyond remains unfunded, but we have secured $5,000 towards the costs of the first step of the plan in 2023: a global stakeholder consultation, with support from the National Institute for Health and Care Research (UK) and the Elsevier Foundation. We still need $7,000 to cover the costs of the work ahead and invite co-sponsorship and donations. We have technical support from JBI (formerly the Joanna Briggs Institute) and the Evidence for Global and Disaster Health group of the International Federation of Library Associations, and we are delighted to be part of the Evidence Based Health Care Day 2023 committee. The centrepiece of the consultation is a global survey, targeting all stakeholders — including and especially publishers —which launches today and runs through to 30 September. Our goal is to demonstrate massive public support for universal access, and to gather inputs from all stakeholders on how to accelerate progress and what more WHO can do. Our target is 10,000 responses.
Misinformation and disinformation are clearly huge challenges to everyone in what you call the “global evidence ecosystem” — what do you see as publishers’ role in addressing them?
Much has been written about different approaches to misinformation. I think a starting point is for publishers, especially those that publish healthcare information, to recognize that they have a responsibility to do everything they can to ensure that people have access to the information they need — information that is reliable, relevant to their context, in the right language, and applicable. This includes both working to reduce misinformation, and also to empower people to differentiate between reliable information and misinformation. This should be part of every publisher’s DNA.
Where else can/should publishers get involved?
To date, the only stakeholder group in the global evidence ecosystem to explicitly commit to universal access to reliable healthcare information are doctors, through the WMA. Several individual publishers have officially supported this goal, and we have welcomed them as HIFA supporting organizations. Cochrane, a HIFA-supporting organization and publisher of systematic reviews recently published a Call to action: supporting evidence responses to global health emergencies for more commitment and investment in reliable information, especially evidence syntheses, in global health emergencies. HIFA is one of the 12 signatories and we have offered to collaborate, pointing out that there is a bigger issue here: we call for greater commitment to improve the availability and use of reliable healthcare information for all health decision-making, from the home to the health facility to the policymaker.
Which publishers are you currently collaborating with, and why? How are they engaging with your work, and are there opportunities for other publishers to get involved?
In 1994, the BMJ and INASP, and specifically Richard Smith and Carol Priestley, introduced me to the world of improving the availability of healthcare information. BMJ’s Fiona Godlee and most recently Kamran Abbasi have also been very supportive and we have a BMJ representative on our steering group. Richard Horton of The Lancet, likewise, has been a longtime supporter and we now have a Lancet representative on our steering group too. We have published several papers in both BMJ and Lancet journals. Our supporting organizations include several journal publishers, as well as publishers of practical manuals such as the wonderful Hesperian’s Where There is No Doctor (a must-have for all health workers — including doctors — working in very low-resource settings).
We invite all publishers to join our forums (English, French, Portuguese, Spanish) and/or apply to become a HIFA supporting organisation.
What about the wider community – are there ways that, for example, libraries, funders, and others can support your work?
Yes, I would encourage everyone to join HIFA (it’s free) and please also complete our global survey (open through September 30) — we are seeking inputs from everyone in the global evidence ecosystem, and that includes patients and the general public. Help add your voice to call for concerted action to improve the availability and use of reliable healthcare information. Contact me if you have any questions or would like to collaborate: neil@hifa.org
Discussion
4 Thoughts on "Universal Access to Reliable Healthcare Information: An Interview with Neil Pakenham-Walsh of HIFA"
HIFA has always been an excellent example of an international network bring professionals from over 100 countries. The coordinator is the best to speak on HIFA’s objectives and achievements. The interview questions and the answers respond clearly to the cause of Health Information for All, which is, I think, is a prerequisite for Universal Health Coverage (UHC). There will be no universality unless people (patients, no-patients, families, health workers) have the knowledge to support their health status.
HIFA is a best platform to share knowledge, discuss the ideas and public policies on reliable health care information as the network is spreading over the globe with all types of stakeholders. It needs to be streghtenged and recognized as a supporting Health Information Institution by the WHO and local country authorities to provide reliable information to achieve SGG- 3.
Thank you Najeeb, HIFA greatly appreciates your ongoing support as a former director of Knowledge, ethics and research at the World Health Organization. WHO defines universal health coverage as ‘all people have access to the full range of quality health services they need’, and ‘Quality of care is the degree to which health services for individuals and populations increase the likelihood of desired health outcomes’. Universal health coverage, quality of care, and desired health outcomes are all inherently dependent on the availability and use of reliable healthcare information, and the ability to differentiate such information from misinformation. This applies at all levels of care (and prevention) from the home and community through all levels of the health system. As you say, there will be no universality until every person has access to the healthcare information they need. To achieve this, there is an urgent need for high-level support for universal access to reliable healthcare information. The surest way to secure such support is to demonstrate public support and solidarity. I urge all readers to add your voice by completing our 5-minute survey: http://www.hifa.org/survey2023 And please invite everyone you know to do the same!
Thank you Murali Prasad,
“It [HIFA] needs to be strengthened and recognized as a supporting Health Information Institution by the WHO and local country authorities to provide reliable information to achieve SGG- 3”
Yes, we are now recognised as an NGO in official relations with WHO. As I mentioned in the interview, we have an agreed collaboration plan with WHO [ https://publicspace.who.int/sites/GEM/official_relations_details.aspx?id=1442 ]. HIFA alone is responsible for raising the funds for this collaboration. Unfortunately we lack fundraising expertise and have not been as successful in fundraising as we have with all other aspects of our work. So the collaboration with WHO remains unfunded – it exists on ‘paper’ only. I invite readers to contact me if they can help or have suggestions: neil@hifa.org
On the point “to provide reliable information to achieve SGG- 3”, the primary remit of HIFA is not to provide healthcare information but to bring people together to explore the many issues and challenges relating to the availability and use of information and how these can be addressed. As WHO said at the launch of HIFA: ‘Healthcare information for all is an ambitious goal but it can be achieved if all stakeholders work together’